What Goes Into Diabetic Eye Care?
Have you been diagnosed with diabetes? Uncontrolled blood sugar levels can affect many parts of your body, including your eyes.
If you have too much glucose in your blood, it causes damage to the tiny, fragile blood vessels in the retina. As a result, this can cause vision problems and even lead to permanent blindness.
Fortunately, regular eye exams and various lifestyle changes can help manage diabetes and protect your vision. Keep reading to learn more about diabetic eye diseases like diabetic retinopathy and tips for maintaining your best quality vision.
What is Diabetic Eye Disease?
Diabetic eye disease is a group of eye conditions that can affect your vision when you have diabetes. These include diabetic retinopathy.
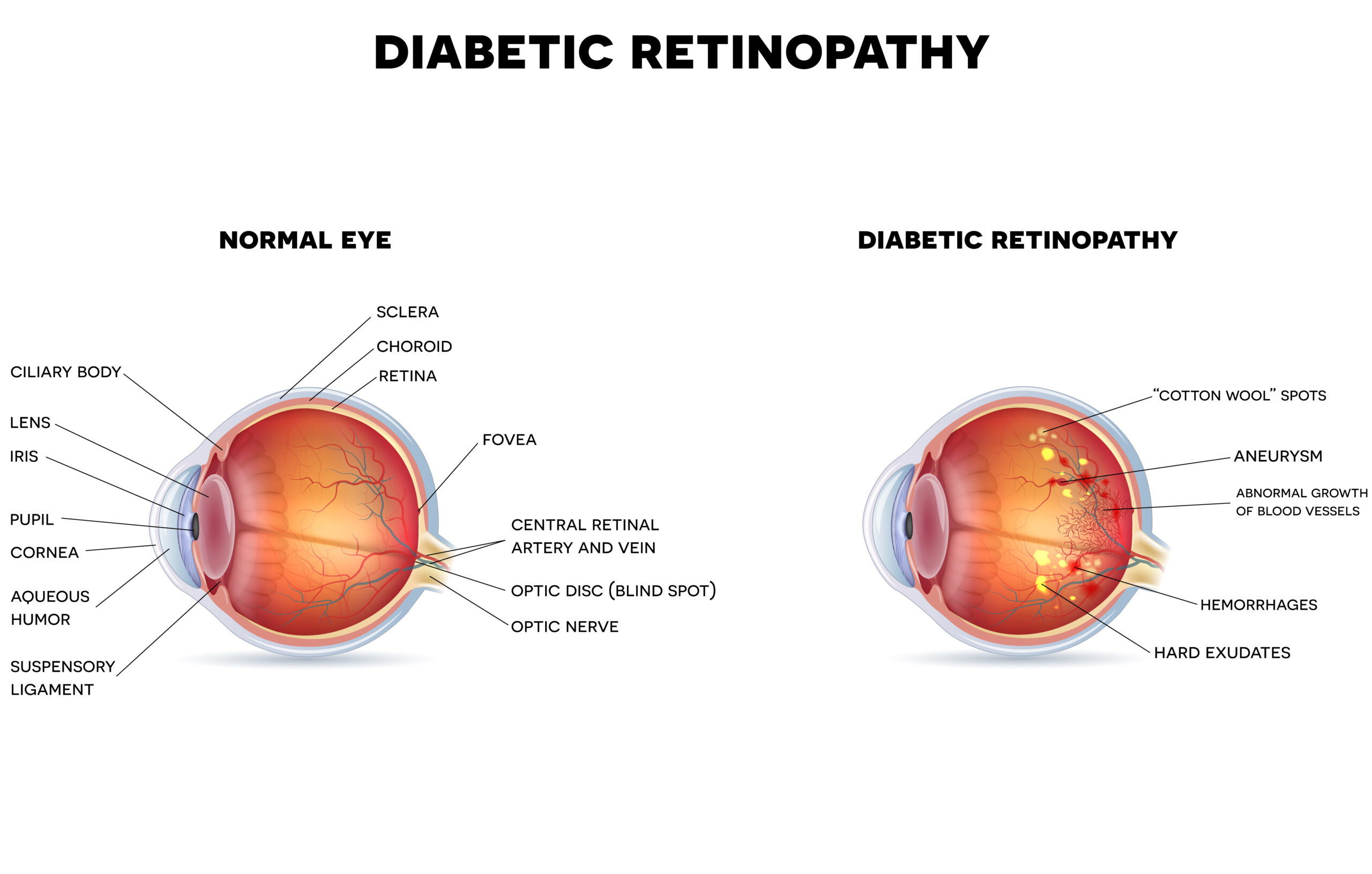
Diabetic retinopathy occurs when excess blood sugar affects the blood vessels in your retina. The retina is the membrane at the back of your eye that sends light signals to the brain, which is essential for vision.
When elevated blood sugar damages small blood vessels in the retina, it causes them to bulge by forming microaneurysms. The microaneurysms leak blood and fluid into the retina. Due to this, you’ll experience blurred vision, distortion, and blind spots.
You may start growing new blood vessels to replace the damaged ones. However, these new blood vessels are fragile and leak more easily.
Growing new abnormal blood vessels is a stage of diabetic retinopathy called proliferative diabetic retinopathy (PDR). Proliferative diabetic retinopathy is a more advanced stage of diabetic retinopathy.
Diabetic retinopathy typically affects both eyes. As it progresses, you may have the following symptoms:

- Blurred vision
- Floaters
- Fluctuating vision
- Poor night vision
- Impaired color vision
- Streaks or patches that block your vision
- Empty or dark areas in your vision
- Sudden and complete vision loss
Although there is no cure for diabetic retinopathy, early diagnosis and prompt treatment can help preserve your remaining vision.
Complications of Diabetic Retinopathy
When left untreated, diabetic retinopathy can lead to complications like:
1. Early Onset Cataracts
When blood sugars fluctuate, there are temporary changes in the natural lens of the eye that cause large shifts in focus. Eyeglasses prescriptions will change dramatically and over time, the natural lens inside the eye becomes cloudy.
In patients with diabetes, there is early and rapid formation of a specific subtype of cataract, known as a posterior subcapsular cataract. Elevated blood glucose levels are a major risk factor for the early development of posterior subcapsular cataracts.
Posterior subcapsular cataracts develop at a rapid pace and can quickly degrade your quality of vision in a matter of several weeks or months. Symptoms of diabetic posterior subcapsular cataracts include blurred vision, glare, halos, and poor night vision.
2. Macular Edema
Located at the very center of your retina is the macula. It’s responsible for your sharp, central, straight-ahead vision.
Macula edema refers to the swelling of your macula. In diabetic retinopathy, macular edema happens when fluid leaks from the damaged blood vessels into your macula.
Some of the symptoms of macula edema are blurry vision and blind spots in your central vision. Loss of vision from macula edema can range from mild to severe.
However, your peripheral vision will be functional, even in severe cases of macular edema.
3.Vitreous Hemorrhage
The new, fragile retinal blood vessels that grow in proliferative diabetic retinopathy can leak blood into the vitreous. The vitreous is the gel-like fluid that fills your eye.
If bleeding in the vitreous is mild, it can cause a few floaters. But when it’s severe, you may suffer nearly total vision loss.
Tractional Retinal Detachment
As the new blood vessels linked to proliferative diabetic retinopathy continue bleeding, they can start to form scar tissue. They may also contract or shrink.
If the blood vessels contract, it may pull on your retina, leading to retinal wrinkling and vision distortion. Too much shrinking of these blood vessels may cause a pull on your retina that’s strong enough to cause a tractional retinal detachment.
Without prompt treatment, tractional retinal detachment often results in complete blindness.
Neovascular Glaucoma
Sometimes, the abnormal blood vessels in proliferative diabetic retinopathy may start forming on your iris and in the drainage channel in front of your eye. If this occurs, it can prevent fluid from flowing out of your eye.
Without an opening for fluid to drain, your eye pressure can increase and cause neovascular glaucoma. Neovascular glaucoma leads to severe eye pain and optic nerve damage. If the pressure isn’t controlled, there may be irreversible vision loss.
Diabetic Retinopathy Treatment
Diabetic retinopathy treatment will depend on various factors, including the severity of your condition. During the early stages, your eye doctor may monitor diabetic retinopathy and recommend lifestyle changes like maintaining blood sugar levels.
Keeping your blood glucose levels under control can greatly slow the progression of diabetic retinopathy. Your ophthalmologist may want to see you for comprehensive eye exams every few months.
Treatments like Anti-VEGF injection therapy can also be used when diabetic retinopathy has progressed. Anti-VEGF injections are medications that help prevent the growth of new, abnormal blood vessels.
However, if diabetic retinopathy is very advanced, surgical intervention may be necessary.
Tips for Diabetic Eye Care
As a patient with diabetes, you may be able to preserve your remaining vision with the following tips:
Scheduling Regular Diabetic Eye Exams

Damage to the eyes due to diabetes is not always noticeable at first. But once you experience changes in your vision, diabetic retinopathy may have already started progressing.
As diabetic retinopathy progresses, the risk of experiencing permanent vision loss increases. For this reason, patients with diabetes need to schedule annual eye exams before experiencing any signs of vision loss.
Early detection and prompt treatment are critical in preventing irreversible vision loss.
Keep Your Blood Sugar and Blood Pressure in Check
High blood sugar and blood pressure can severely damage the blood vessels in your eyes and impair vision. It’s crucial to monitor and control your blood sugar and blood pressure.
You can enjoy good vision for years to come with proper blood sugar and blood pressure management.
Focus on Eating Healthy

Maintaining a well-balanced diet can help control diabetes and blood pressure. Ensure you consume eye-healthy foods packed with vitamins A, C, and E, lutein, zinc, beta-carotene, zeaxanthin, and omega-3 fatty acids.
You can attain this by eating fatty fish like tuna or salmon, colorful vegetables and fruits, mushrooms, beans, lentils, and nuts like almonds and walnuts.
Protect Your Vision from Diabetes
Do you have diabetes? Be proactive about your vision by scheduling a consultation at Desert Vision Center. Dr. Tokuhara is highly experienced in diagnosing and treating diabetic eye disease.
Request your consultation at Desert Vision Center in Rancho Mirage, CA, now!

